Hormone Therapy: The Study That Changed Everything (And the Science That Followed)
- Nicole McGann

- Jan 27
- 2 min read
How Hormone Therapy Went from Routine to Risky Overnight
For decades, doctors had been prescribing estrogen and progesterone for “menopause transition” symptoms. Then in 2002, a study by the Women’s Health Initiative (WHI), funded by the National Institutes of Health (NIH) - the largest, most expensive women’s health study ever conducted shared its findings:
•The combined estrogen + progestin group showed a small absolute increase in breast cancer
•The estrogen-only arm (women without a uterus) did NOT increase breast cancer risk
•In later follow-up, estrogen-only therapy showed lower breast cancer incidence and mortality
The Findings Translated Publicly to:
Hormone therapy increased breast cancer Hormone therapy increased heart disease Hormone therapy increased stroke Hormone therapy increased blood clots
what the world heard "Hormone replacement therapy causes cancer!"
Women stopped taking it en masse and menopause care froze for 20+ years.
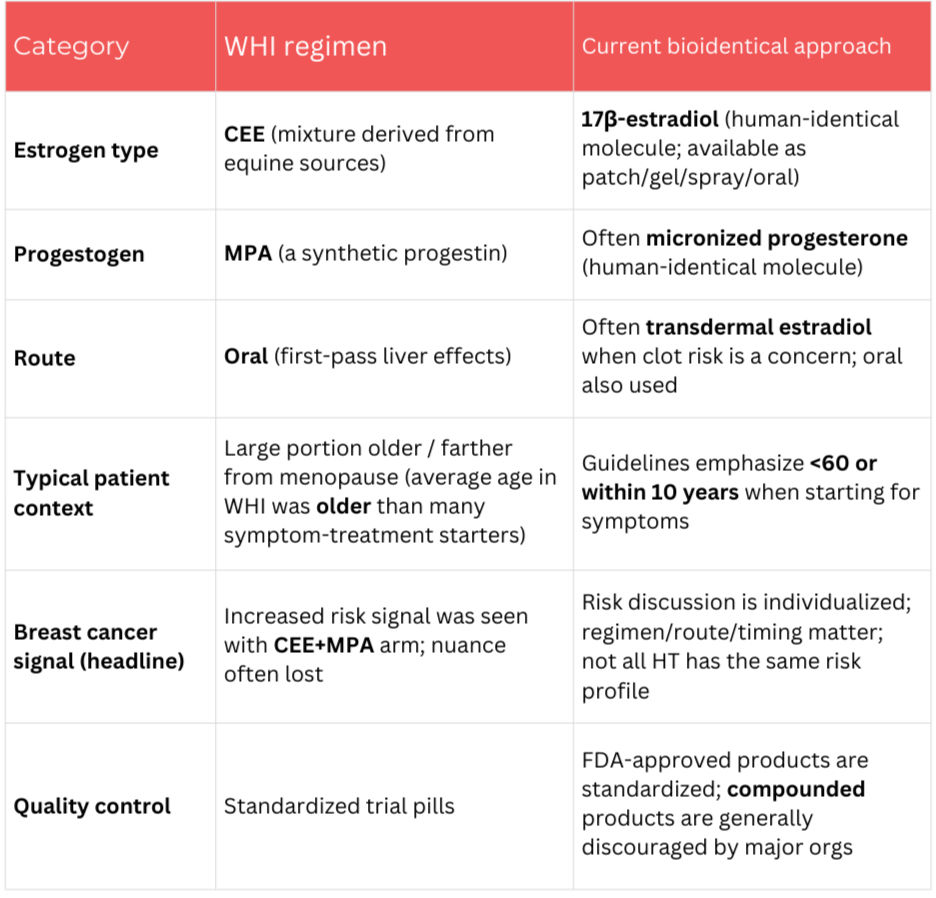
Over the Following Decade, Scientists Came to Understand
Timing matters
Formulation matters
Route matter
Combining hormones matters This led to the “timing hypothesis” and major guideline revisions—but without a public reckoning as loud as the original scare.
Key Takeaways
Here's what leading women’s health organizations and practitioners now believe is important for safe and effective administration of hormones for relief of perimenopausal symptoms:
AGE:
Women should be ~60 years old or within 10 years of menopause onset. (1)
APPLICATION:
Estrogen patches or gels are less likely than pills to cause blood clots and stroke (1)
HORMONE FORMULA:
17β-estradiol is preferred over conjugated equine estrogens because it is chemically identical to human estrogen (1)
Micronized progesterone is preferred over synthetic progestins because it protects the uterus lining and has fewer side effects (2)
HORMONE PAIRING:
If you still have a uterus, estrogen must be paired with progesterone to prevent the uterine lining from building up and raising the risk of uterine cancer. (1)





Comments